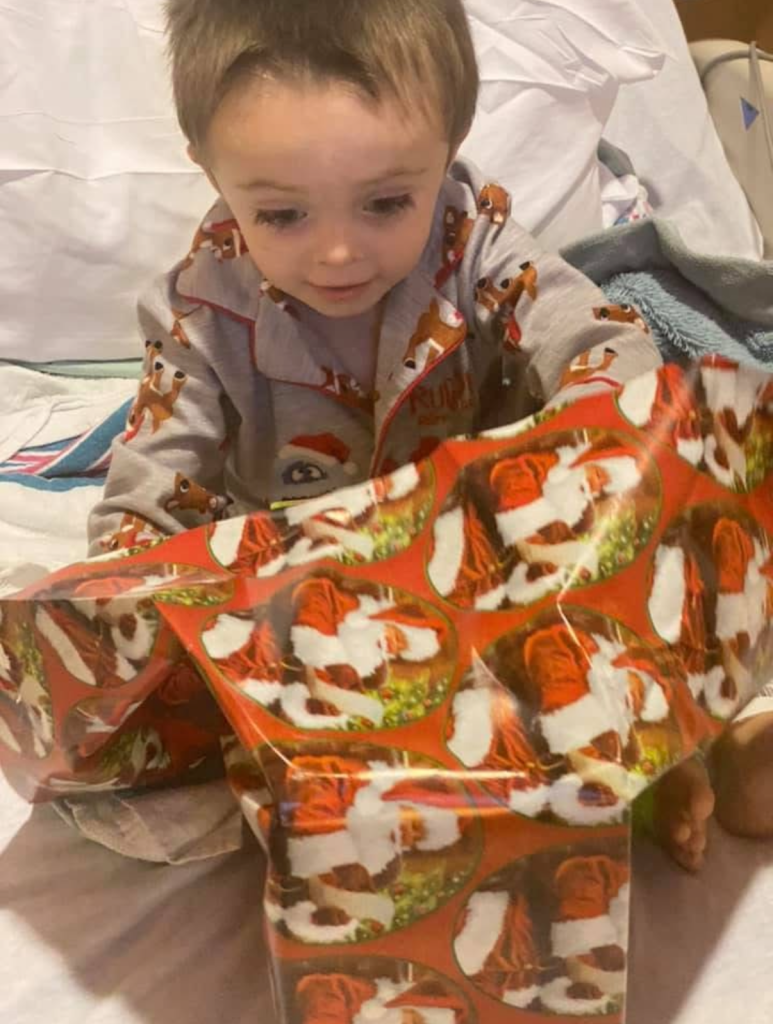
December 2020, while going to get tested for covid before Christmas, we took Christian to his pediatrician to get tested. While performing his examination, the nurse said that he had diminished chest sounds on his right side of his chest and that we should take him to the emergency room for an x-ray. We left his doctor’s office and headed to Orange Regional in Middletown because we were supposed to get a snow storm this night and wanted to be closer to home. Because of covid at the time, they would only let one parent in at a time. Tracey went in with him while I sat in the car with our other two children. While inside, they performed an x-ray and said that they believed he had pneumonia and wanted to transfer him to Maria Fareri Children’s Hospital in Westchester. They transported Christian and Tracey by ambulance down to Westchester. I headed home. Once Christian and Tracey arrived to Maria Fareri, they sprayed a medicine up his nose to try and calm him down so they could perform a CT scan. After the CT scan, Tracey was informed that he didn’t have pneumonia, he had a tumor in his right chest and fluid build-up. I immediately headed for the hospital. The next morning, they took Christian for a biopsy. While taking the biopsy, they ended up draining a liter of fluid from his chest and placed a chest tube. A little while later our oncologist came to see us and discuss the results of the biopsy. He told us that the tumor was a rare form of childhood cancer called Pleuropulmonary Blastoma or PPB for short. PPB is a very rare childhood cancer that less then 50 kids a year in the US of diagnosed with. There is very little research on the disease. We were told that his was type 3 which is a solid tumor type of PPB. Our oncologist told us that he was actually one of the lead doctors on the PPB registry trying to study more about this cancer and working on a cure. The current recommendation at the time for treatment consisted of chemo therapy, surgery, and possibly radiation. In order to give the chemo meds, Christian needed a central line placed. They implanted a central line in his left arm. The next day his entire hand to swelled and they were unable to get any blood return from the line so they were unable to use this line. They had to remove this central line and decided to implant a Broviac catheter. A Broviac is a set of tubes that stick out from the center of your chest that is connected into a large vein in your chest allowing for fast access to blood draws, administering chemo meds, and fluids. Chemo therapy started right away which consisted of several chemo medicines that were given over the course of 2 days in the hospital. We spent 4 weeks in the hospital before being discharged. Over the next several months, Christian was given 7 rounds of chemo meds to ensure the tumor was reacting to the meds before they could attempt surgery. The hope was to shrink the tumors as small as possible before removal through surgery while still leaving enough rounds of chemo post-surgery to kill any remaining cancer cells. April of 2021, everyone agreed it was time for surgery. His surgery consisted of the removal of his entire plural wall lining in his right chest cavity and the removal of his upper lope of his right lung. His surgery took six and a half hours to complete. He came out of surgery with a chest tube placed to help drain any remaining fluid from his chest. After surgery he recovered in the PICU for several days before being transferred down to the normal floor. For the first few days after surgery, there was an air leak in his lung that they could see in the container for the chest tube that showed up as bubbling within the fluid in the container.




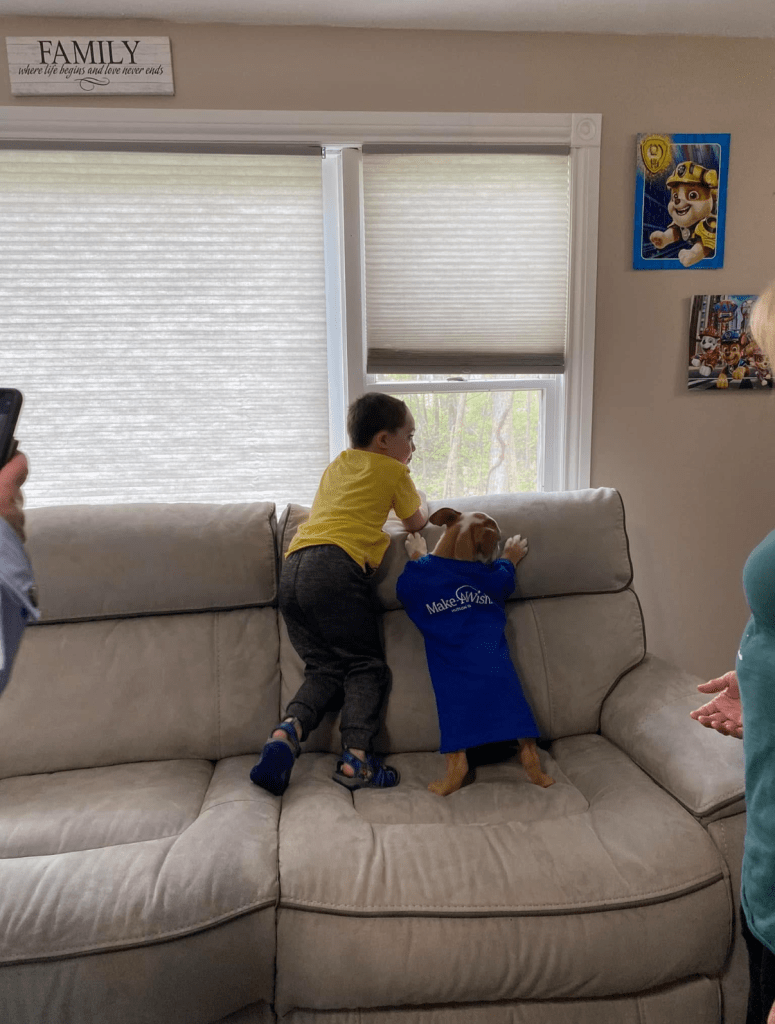
Post surgery, he developed a fever and cultures showed several organisms growing from his Broviac. After about 4 days of this air leak, they decided to go back in to remove the Broviac due to his fever and to try and patch the air leak. After the air leak continued, they decided to try and stop the leak by pushing a platelet type fluid into the chest through the chest tube and laying him on his side for 15 mins and then rolling him over for 15 mins. This was an attempt to glue the hole within the stitches in his lung. This proved unsuccessful. He remained in the hospital for 3 weeks with the chest tube in place. One day while the custodial staff was cleaning his room, we believe they accidently snagged his chest tube line and pulled it out. After they left from cleaning the room, I got up and noticed the end of the chest tube laying on the floor no longer in his chest. I immediately ran out to grab a nurse who rushed in and installed a patch cover over the chest tube hole. The doctors came shortly after and were concerned the lung would deflate without the chest tube being in place so they scheduled an x-ray. The x-ray actually showed that the lung volume increased after having the tube pulled out. We were discharged from the hospital 3 days later. This entire hospital stay was 4 weeks. After two more weeks home recovering, he had to have a new central line placed so they could continue chemo so they decided to implant a under skin chemo port. He then began his chemo treatment again. He completed his twelfth and final chemo cycle of his chemo treatments at the end of October of 2021. In March of 2022 his chemo port was removed. Each of the twelve chemo cycles consisted of the following, beginning on Fridays as day one of week one of a three-week cycle, day 1 = 1 dose of Vincristine, 1 dose of Actinomycin, 1 dose of Ifosfamide, twenty hours of Mesna starting with the Ifosfamide, and 1 dose of Doxorubicin, day two = 1 dose of Ifosfamide, twenty hours of Mesna starting with the Ifosfamide, and 1 dose of Doxorubicin. After being discharged from his two days of chemo, we had to give him a GCSF shot at home 24 hours after his last chemo med. During these 12 cycles they performed several scans that included full body bone scans, brain mri’s, and chest CT scans. While having his chemo port and Broviac, at any time if he ran a fever, it meant having to rush to the emergency room where they would take blood cultures to be tested for infection before giving two courses of antibiotics 24 hours apart. With having the under-skin chemo port, it has to be accessed either in the hospital or clinic at least once a month and flushed with saline and heparin to prevent blood clots from forming at the tip of the line in the vein. While having his Broviac implanted, we had to flush both lines with saline and heparin every night at home. We had a nurse come to the house to show us how to flush. Keeping the Broviac clean takes a lot of work but it’s absolutely the most important part about having the Broviac. You have to keep the site clean and dry, which means no baths for children so we had to wipe him down with CHG wipes and give him sponge baths and cover the are with bandages during that time to keep it dry and from getting an infection. In November, Christian’s wish from Make-A-Wish was granted and he received an English Bulldog that he named Rubble.