







On December 22nd, 2023, because we tried to see if he would do his three-month follow-up scans awake, but he was not ready to do so and that was perfectly fine. We completely understand how scary it can be having to go into these big machines and must sit still even tho we can be in the room with him holding his hands right by his side. This ended up delaying these scans by about a week. On Dec 28th, 2023, we went for Christian’s three month follow up scans which consisted of a full body bone scan, brain MRI and CT chest. To do all three scans at our home hospital in one day would take about five hours just for scans and he would be under anesthesia the entire time. On this day he started at 8am. They usually call with updates when they get to the next scan to let us know how he is doing. They called said he was in nuclear medicine then time kept going by and no call, we started to panic. I asked the receptionist to call see how he is doing but didn’t get a straight answer. Some more time went bye I asked again. I then went into the back recovery area to ask a nurse who told me they would find out and let me know. I went back to waiting area but still no update. I went back to the nurse’s station again and finally emailed the oncology office to see if they knew what was going on or if they had an update. They called and said he was going for an x-ray, but he was not scheduled to have an x-ray during this set of scans, so we knew something was not right. They told us that his oncologist was in the hospital and would come talk to us. My anxiety was through the roof. Our son’s oncologist walked in the waiting room, I said “is it bad?” he said lets all go talk in a private room. I couldn’t hold back the tears at this point. He sat us down and said that he sees what he was sure was a tumor, a very large tumor on his right lung by his heart and on his diaphragm pushing into the liver. His past follow-up scans showed a spot on the diaphragm, but they thought it was just scare tissue. He was having no symptoms. This would be his second relapse. The doctor didn’t have many answers at that moment. They brought our son into recovery and did a chest x-ray. When he woke up, like always, I would get into the bed and hold him. His doctor said he wasn’t going to keep us for New Years as he didn’t want to ruin another holiday for us, but we didn’t care, we just wanted him better. Before we left the hospital his doctor said he would do some research and talk with the registry and try to come up with a plan. Up to this point, he has already had all the standard treatment for PPB. He also gave us the option to let the tumor take over and keep him comfortable if we didn’t want to put him through treatment and surgeries again. This was NOT an option for us; we would go to the ends of the world to find a cure and get him help to get better. When hearing that as a mom or dad, your body goes numb, and the heart break is unreal. We left the hospital that night scared to death, unless you’ve been through this, no one could ever understand the pain and fear a parent, child, and sibling goes through in a time like this. Not having answers is even scarier. PPB cancer is so rare that twenty to fifty kids get it a year in the world. It’s even rarer that it comes back for a second relapse. We went home tried our best not to cry in front of him the next day we called his surgeon to see what his thoughts were and what he could do to help. I tried to go into work but just couldn’t. This was the day I stopped working and stayed home with my kids. The surgeon called and said to us that looking at the images, he didn’t think there was anything he could do, that surgery would be too risky and that he wanted to see what his oncologist comes up with. We told him the same thing whatever we must do to keep our son safe and healthy, that giving up was not an option for us. He knew that already just dealing with us the last go around. The same day we went to round one arcade, one of his favorite places to go. The next day we went to big snow in the American Dream Mall because he had been wanting to go slay ridding and we still didn’t snow by us. Not knowing what the next days were going to bring, we wanted to do as much fun stuff for him and try and make as many happy fun memories as possible. Christian and his sister had an absolute blast. His sister kept positive and strong throughout this whole time. The next day we celebrated New Year’s Eve at home. Jan 2nd, we went to MSK in the city for more scans under anesthesia and to meet with his surgeon. The news we got from the surgeon was not good. He said every time it comes back, it’s more complicated for surgery, and that he needs to see that chemo will shrink it before he would talk about doing surgery. He said there would be no point in putting him through surgery if the tumor wasn’t responding to the chemo. If it does shrink, it will be very risky to do surgery. If he was to make it through, he would very likely be in a ventilator for a while. If during the surgery they found that theTumor was attached to heart, they would have to stop and wouldn’t be able to perform the surgery. The tumor was pushing through his diaphragm into his liver and surrounded his middle lobe of his lung. When this cancer starts, its very aggressive and can spread very fast. It was also touching the bag around his heart. We asked the doctor if he going to be ok and he just went silent before saying I can’t say that he will be. January 4th, we had appointment with the oncologist to discuss what he came up with for treatment options so we could determine what type of chemo port he would need to have placed. The first option he gave us was to just keep him home and comfortable because this is the third time it has came back and instead of possibly putting him through hell for the outcome to be the same, we immediately said no to this and told him this will never be an option. The second option was a chemo regimen that he came up with that helped other kids with different solid tumors that shared similar cancer genes, so we agreed to go with this option. Thank God his oncologist came up with this regimen for other kids with solid tumors as it is in trial still. This time there was nothing on file with the PPB bored registry for a treatment plan.





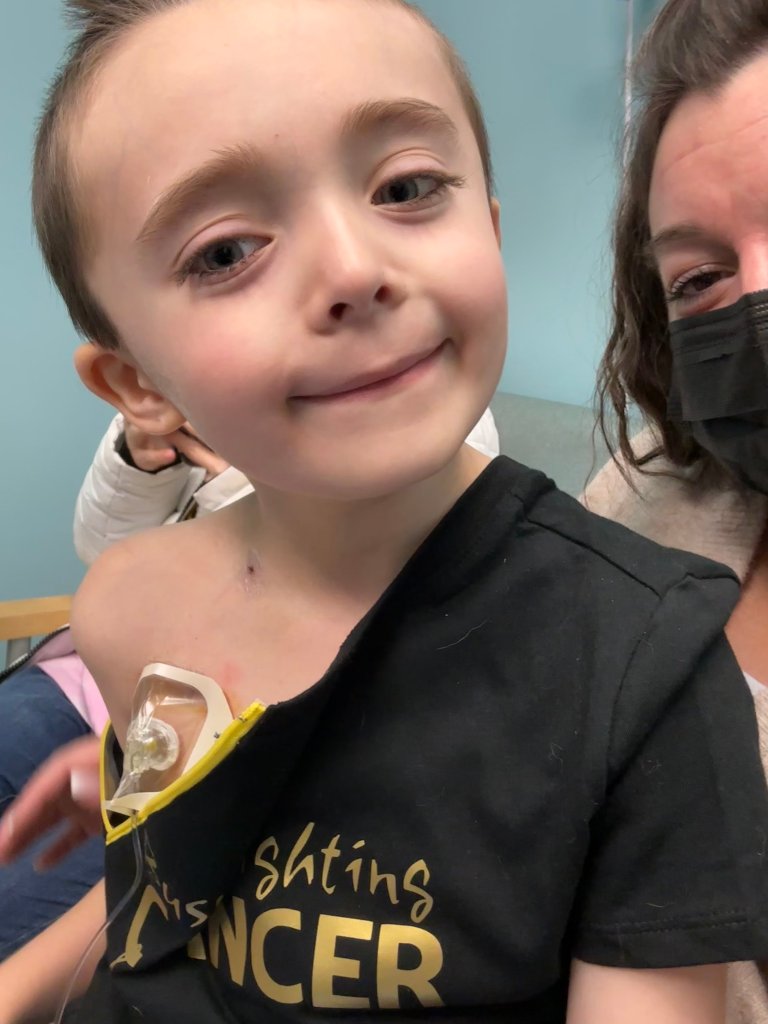





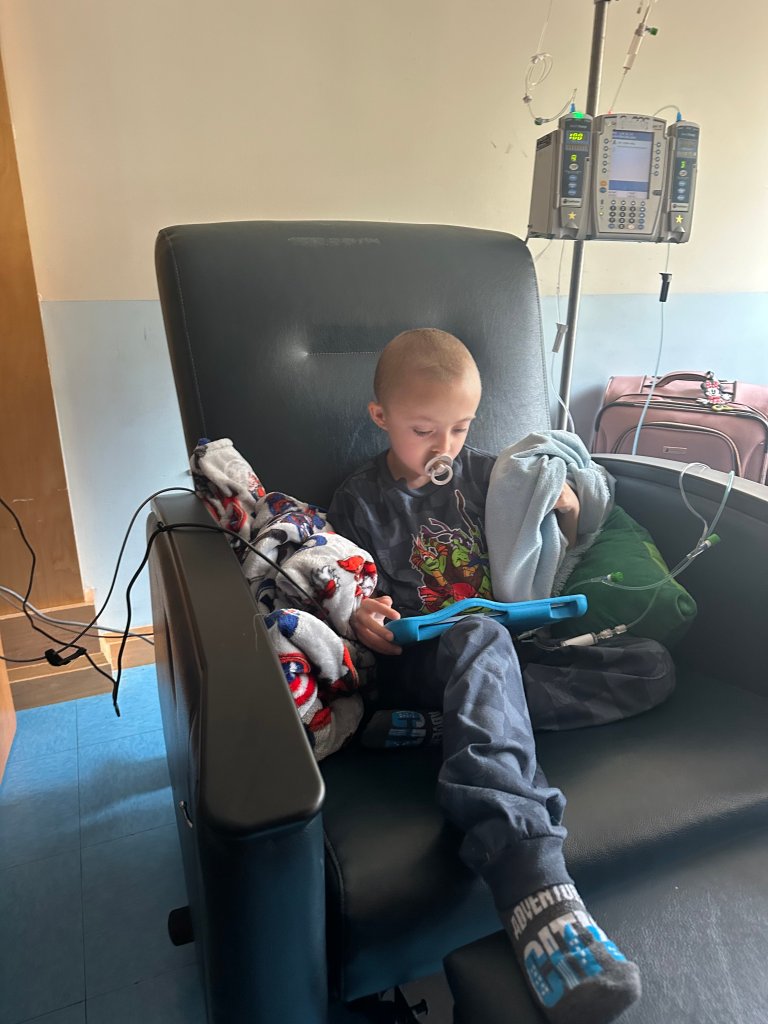
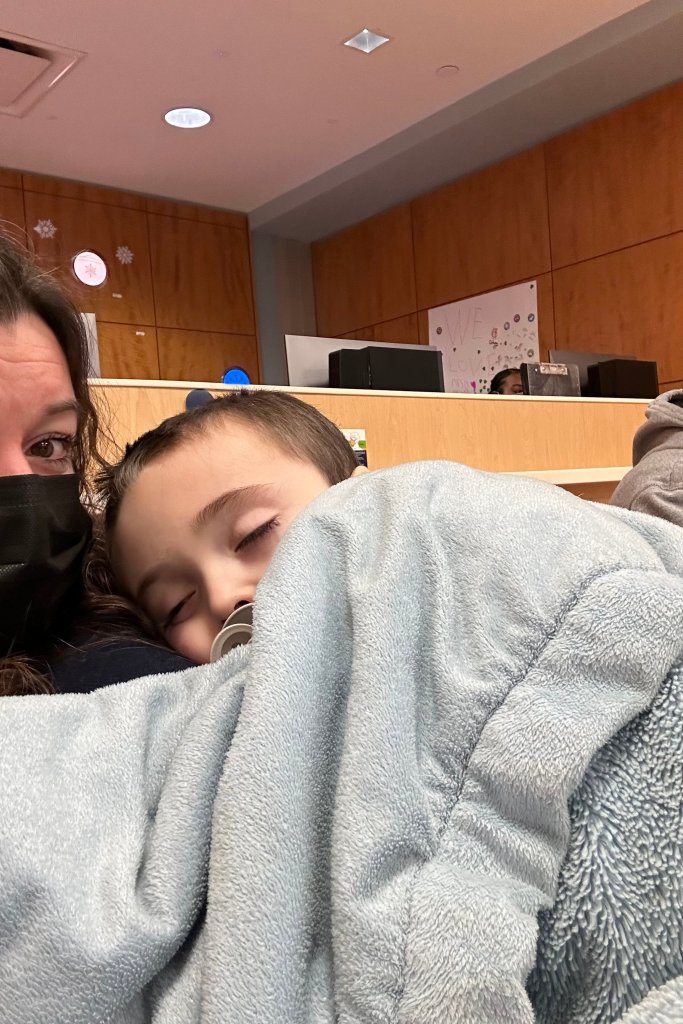
Next, we called MSK to schedule a surgery for him to have another chemo port placed the following Tuesday. We also asked if they could do radiation this go around because that was one thing we didn’t try yet as a part of his treatment. The doctor said no that would make surgery riskier because it does not allow his body to heal properly from the damage that the radiation would do to the surrounding area. January 9th, he was scheduled to have his chemo port placed at MSK. They did an ultrasound to help put the chemo port in because the tumor was so close to his heart. They tried to place the chemo port in on the left side where he had them in the past but couldn’t because the tumor was pushing everything over towards the left side. This one was a single lumen chemo port with a line that goes into his major artery in his neck. We went back to his oncologist office on the Friday after the chemo port was placed for bloodwork and to plan to start chemotherapy on the following Monday. While with the oncologist, we talk about radiation after surgery if surgery was possible. He also talked about stem cell transplant being an option, but the risks are large. The problem with this cancer is that there is not enough research on it because of how rare is is. To watch your child fight cancer, the words heart breaking is an understatement. As with the placement of his last chemo ports, he bruised around the area of the port placement. Christian’s road map for the first three cycles of this treatment, he had to be in patient in hospital to receive this medicine followed by one day in clinic for another does of one of the medicines because it is a trial treatment option. His inpatient treatment was five days of treatment and then three weeks off during which he would go to the clinic to check his blood work counts. Monday January 12th was supposed to be his first day of this new chemo plan. He wasn’t feeling good when we went in the clinic to get clearance for admission. They did bloodwork, an x-ray, and covid swab in office. Covid came back positive, so we were admitted into the hospital for a couple days for antibiotics and chemo got pushed off a week, unless the tumor started to have an effect on him. To begin each cycle of treatment, he would have to take Cefixime, which he took two days before he started chemo and for the entire week of chemo to help with diarrhea, then the his chemo medicines were, two chemo medicines by mouth were Vorinostat and Temozolomide and the chemo meds that were hung on the iv pump were called Vincristine and Irinotecan. He would get all these medicines every day for a week than the following Monday it would be a single dose of Vincristine, then he would have two weeks off. For most chemo patients, they must take a medicine called bacterium on the weekends. This is an antibiotic to help prevent sicknesses like the flu and pneumonia. On January 15th, he was finally able to begin the first cycle of this chemo treatment. The first chemo medicine was by mouth; he did great at taking this one. The second one was hung on the iv-pump machine and ran over an hour. This medicine required blood checks before, during, and after to ensure his body was handling the treatment. The second day of chemo he got sick taking the chemo by mouth and had to take it again. We were discharged on January 20th from Maria Fareri Children’s Hospital. He wanted to go to Dave and Busters, so we ran home got changed and then went to have fun for a little bit while he was still feeling good. He doesn’t like to eat the food in the hospital, so when we got home, he wanted everything from pizza, to hotdogs, and even chocolate. Whenever we were home and he didn’t feel good he wanted his feet rubbed and a pedicure. January 21st, he started not to feel so great. He had diarrhea, which was a side effect from the chemo medicine, so we gave him Imodium along with the medicine to prevent the diarrhea. While at home he wanted lots of cuddles with his puppy and mommy. January 22nd, we went to the oncology office for the chemo that gets pushed called Vincristine and routine bloodwork. He does so good with having his chemo accessed. January 23rd was pedicure day because he still wasn’t feeling good. He was sick all week and wasn’t eating much. He would take three fork full of food and say I’m not hungry. When we saw the oncologist, he said they should of never gave him the Imodium before he had the side effects. He began throwing up, so they told us to give him a laxative and after we did, he went a lot. He was still coughing, they said it could be still from covid, or it could be the tumor affecting him. We were also giving anti-nausea medicine around the clock. The doctor sent in a script to make him hungry. The following Monday January 29th we went for follow up bloodwork. His counts were good, so he didn’t need any blood transfusions. They wanted to do another round of scans after his first cycle of chemotherapy to see if the tumor was responding. Monday January 31st, we went to MSK for a chest CT scan with contrast. It was a little bit of a mess of this day. They accused his port in the IV room upstairs and he did great again. Then we headed downstairs to the CT area. The radiologist said they couldn’t use his chemo port for the contrast because on the last x-ray they had, they couldn’t tell if the tip of the line from the port was placed in the correct location. This meant that they had to place a peripheral IV in his hand while he was awake. This made him very upset, and he throw up a couple times while they were doing it. He was ok after the IV was placed and I held him until he fell asleep before we went back to the CT waiting area. He was a little scared when they were injecting him with the anesthesia. When he woke up, they came and got us, and he was already sitting up in the crib with his arms up ready to go. Then we went back to the waiting room, and he fell asleep on me until the team was ready to see us. When we met with the surgeon after the scan was complete and we told him what took place with the CT department, he was very upset because there was no reason for them to not use his chemo port and all they had to do was call him because he placed the chemo port and he knows it was in the right place. We hoped at this point the chemo medicine is working and shrinking the tumor so they can do surgery. The surgeon had said the tumor did grow a little.




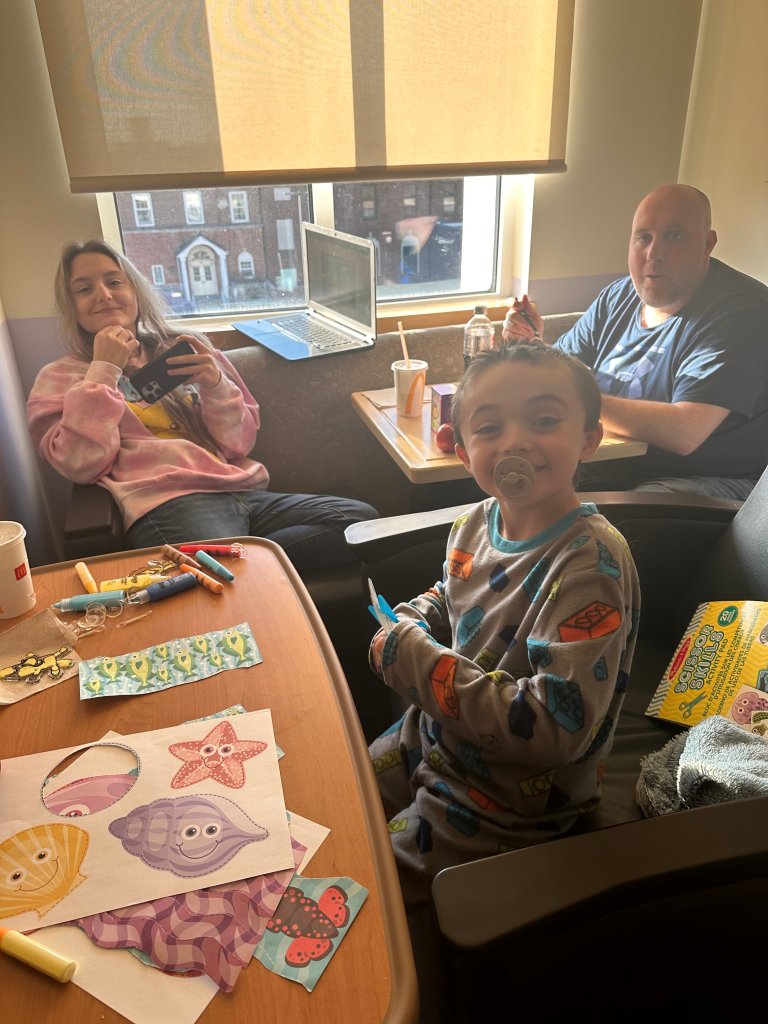

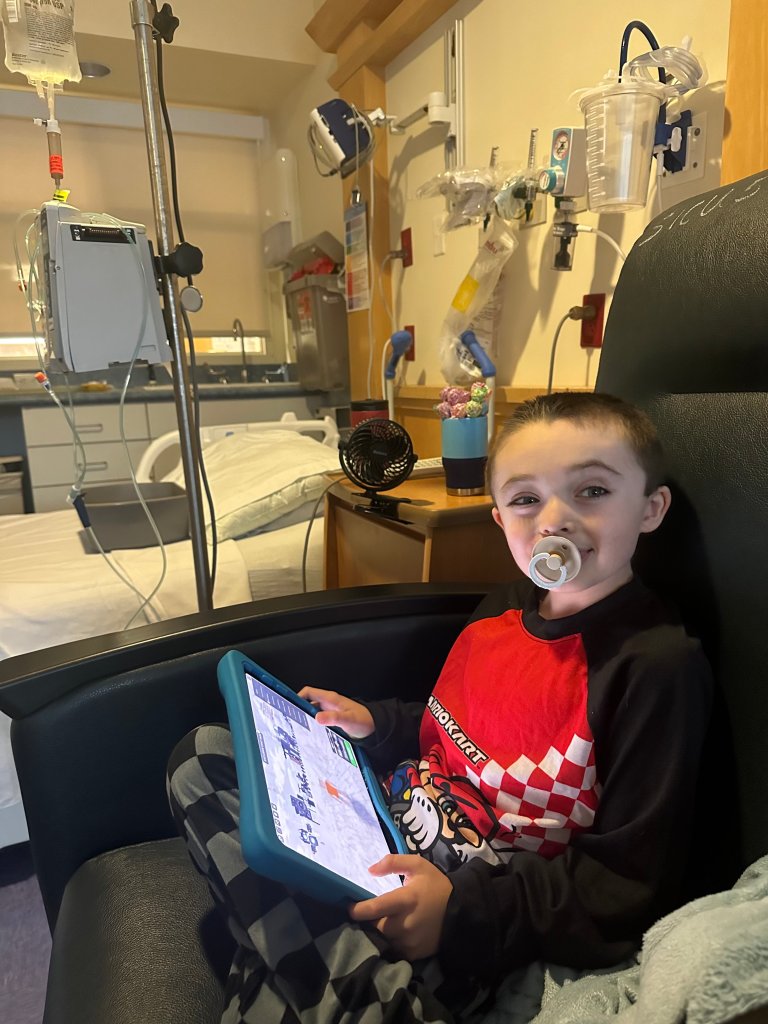




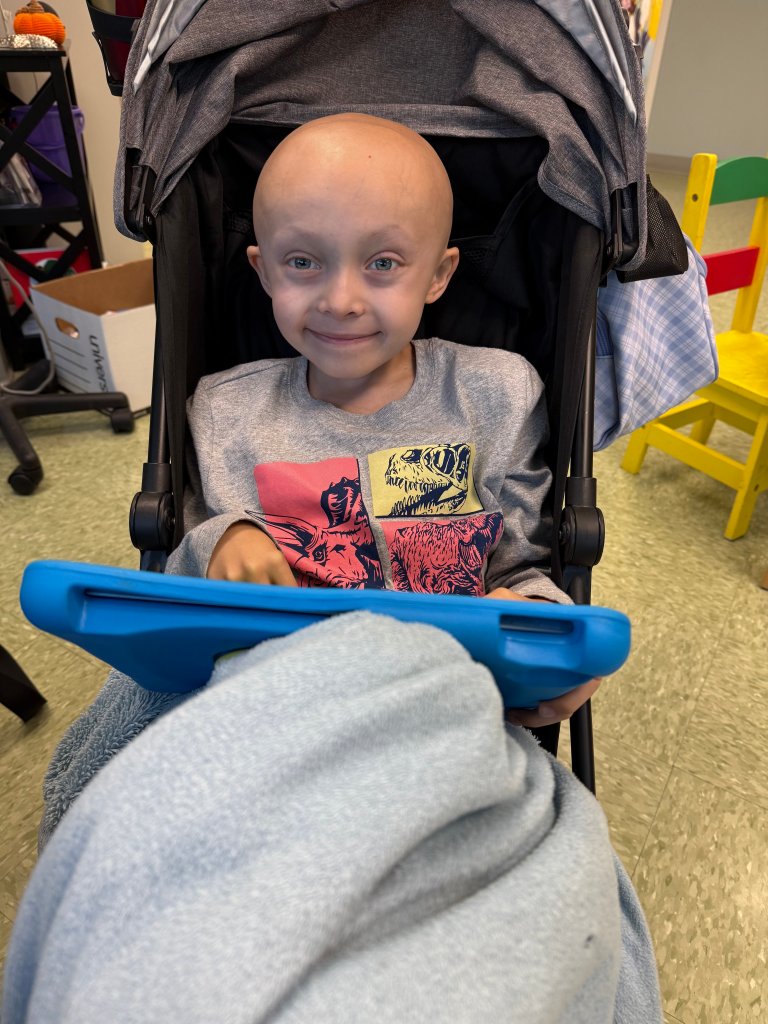
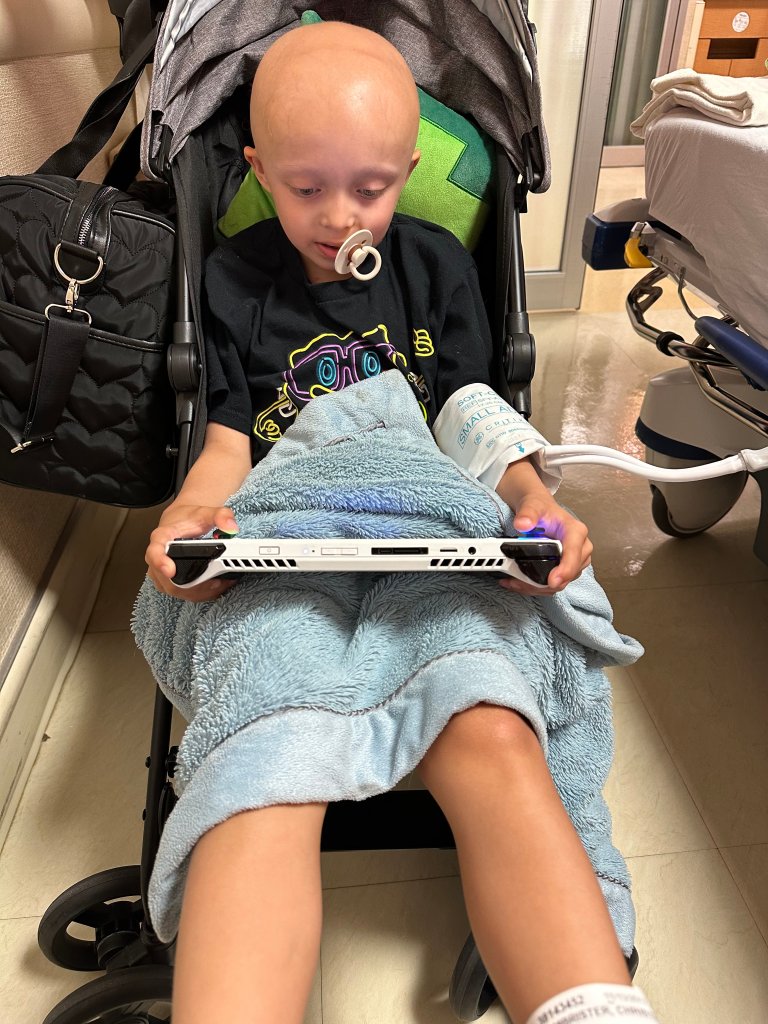
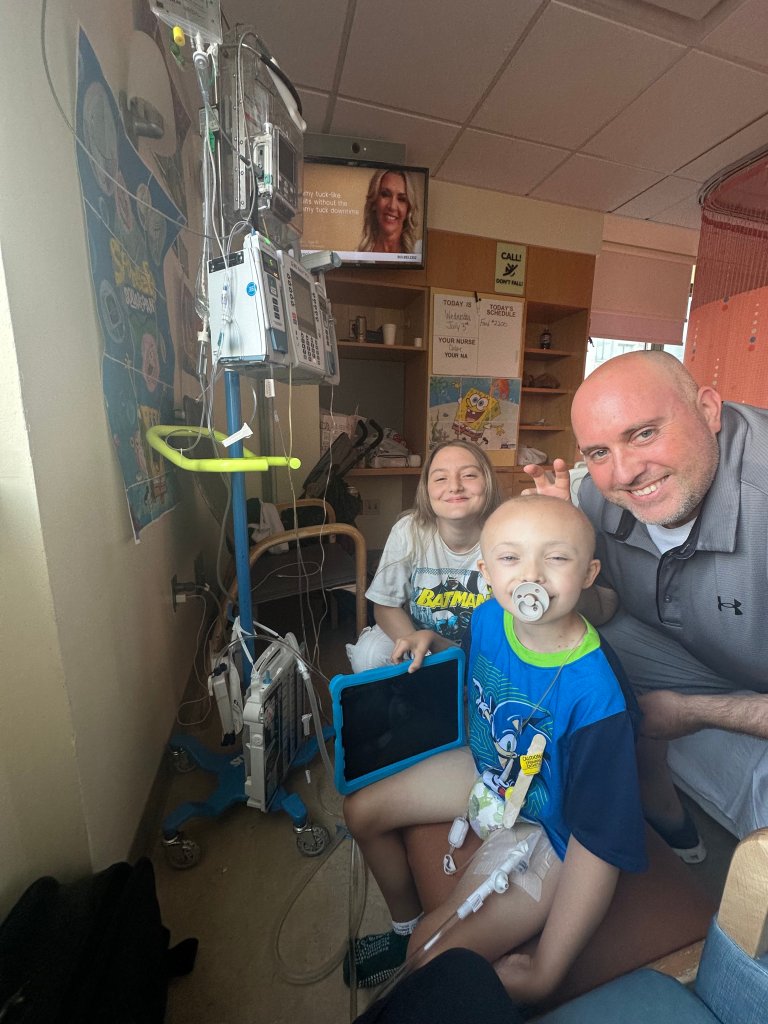
February 1st he was still coughing this was due to having covid. The plan going forward was to do three more cycles of chemo and then repeat scans and at that point talk about surgery. He said it will be a long morbid surgery that every time it comes back, and they have to go in it gets riskier. He thinks he will take out the rest of the middle lobe and lower lobe and then place a silicone implant to keep his heart from flipping. If during his surgery, his heart was to flip, there would be no way of fixing it and that would be it. He also thinks he will take out part of his diaphragm. He said we will have a long intensive conversation when the time comes not to worry about anything right now. There is no way that we can’t worry this, this is our baby, and we are scared to death and don’t want to lose him. The fear and pain I can’t even begin to describe. February 5th, we went to start another round of chemo, but they forgot to order the trial medicine, so we went home and we’re going to go back the next day. The covid swab he did come back positive still for covid. They said it could be because his immune system is compromised, and it can take longer for it to leave his body. He already had the antibody so it will just take time to go away. We would have to quarantine in a room till his covid comes back negative. February 7th we were back in the hospital for the beginning of his second round of chemo medicine. We would bring tons of activities to do from coloring, games, painting, you name it. The second chemo medicine by mouth he got sick again, so we had to wait and do it again. He is so brave for taking it. His hair is falling out at this point, a lot. I know when we go home, and he showers it will mostly all come off. He is ok with being bold. He says he actually likes it better because he looks like his daddy. February 12th we were discharged. The second cycle of chemo he was sick the whole week. This round of chemo he throws up a lot. Because he tested positive for covid we had to stay in his room and couldn’t go to the cafeteria, Panera, the vending machine, or even the gift shop. February 14th, Valentine Day, he went for bloodwork and a chemo push. February 18th, we went to Adventure Aquarium. February 24th, we went to Mystic Aquarium. February 27th we were back in the hospital for another round of chemo. He took the chemo medicine by mouth good and didn’t throw it up. We were discharged March 2nd, 2024. He has scans scheduled for March 12th. The doctor said he doesn’t expect to see much of a change, just as long as it doesn’t continue to grow any bigger, they will know that the chemo is working. At this point in time, they don’t have a set regimen for a second time relapse. They do have one other medicine, but they don’t have a dose for kids under 12. He has had three cycles of chemo before this scan. March 5th we were at the oncology office getting bloodwork and chemo pushed. What I noticed is that this chemotherapy affects him more than the past treatments he has gotten. March 12th, we went to Sloan for more scans and the surgeon said that the tumor has shrunk a little so he is going to talk to the oncologist to see if he will do surgery after the next two or three rounds. He said that the surgery will be a life-threatening surgery but that he also has a life-threatening tumor. Because the tumor is reacting to the chemo, he can do the surgery. If it wasn’t than surgery would not be on the table. He did say there is a chance that he could get in there and have to stop and close him up without being able to take the tumor out depending on what organs and how the tumor was actually attached to everything. The images from the scans only show so much. He said the plan isn’t completely set yet but as of now he thinks he will take everything on the right side of his chest out, a large piece of his diaphragm, and a piece of the bag that surrounds his heart that the tumor is touching. They will do more scans when surgery time gets closer and they have a set plan. He needs to have a pulmonary function test done so they know the left lung is strong. March 18th, he had another round of chemo, but we were able to do it at the oncology office because the trial study for the one medicine was over. Surgery was set for May 23rd with all three scans; full body bone scan, CT chest scan and brain MRI on May 21st. April 8th we went for another week of chemo in oncology office. He was continuing to struggle with taking the liquid med by mouth so this time they had to put an N/G tube in his nose to give him the medicines by mouth. This made it easier for him to take the full doses of the medicine. He did not like getting the N/G tube placed up his nose, but he tolerated it. They would put it in at the doctor’s office first thing in the morning and than we would go upstairs for an x-ray to make sure it was in the right place. It was little hard for him to eat and drink with the N/G tube in place. We would go home with it in all weeks and then they would remove it at the end of the week. One night while we were home, he sneezed and ended up throwing it up and the end came out of his mouth, so my husband had to pull it out from his nose completely. They would give him Ativan that would relax him, and it was also one of the nausea medications. April 8th was the solar eclipse he was sleeping when it happened, but we didn’t want to wake him because he didn’t feel good. Between the chemo and the NG tube. April 18th, we had the father from Our Lady of Fatima Church come to the house to bless him. When we were home and he felt good we played with his cars, bounce house, water balloons, and would go mini golfing. We did everything he wanted to do. April 22nd, he had his pulmonary function test that he did great with. He is so brave and strong its unreal.



April 24th, we went to look at the fire trucks at a local fire station that he was invited to. April 29th was another round of chemo. April 30th, he threw up the NG tube. He was not eating much so we were going to get him his nutrition threw the tube at home, but he would throw up because it was too heavy on his belly. This chemo made him sick a lot. They started talking about putting in a button in his belly when he goes for surgery instead of the NG tube. He was wanting to go to Disney for awhile at this point so we talked it over with his doctors and surgeon to see if it would be safe to take a large trip like that with everything going on. Hi oncologist said yes, absolutely take him to Disney. We discussed together when would be the best time to take this trip to not interrupt his treatment too much. After his next cycle of chemo, we took a trip to Florida. We began the week at the best air show in Fort Lauderdale. We went to Epcot, Sea World where we got to interacted with the dolphins, penguins, and beluga whales. We went to Magic Kingdom, and Universal. We took a day trip Venice beach. While at Magic Kingdom, he lifted the sword out of the stone and was so proud of himself he still talks about it. Leading up to this trip he kept saying that’s all he wanted to do, was show how strong he was by lifting the sword out of the stone behind the castle. May 20th, he had brain MRI at Sloan. We didn’t meet with the team this day, so we left afterwards. May 21st, we went back to Sloan for more scans. When we met with the surgeon, he said looking at the images with the team, it looks like theres a chance the tumor went through the bag and is touching his heart and if this is the case, they can’t do surgery. They set up an MRI for his heart the next day. At this point the chemotherapy has barely shrunk the tumor, so after surgery they are talking about doing proton radiation therapy to the entire right chest. Surgery is the only option to save his life and as of right now there is no other treatment option if it comes back. The CT scan showed an opening where he can cut the tumor from the bag around his heart. The surgeon had said they are planning on taking the rest of the lung, the plural wall again, a part of the bag around his heart and possibly piece of his diaphragm. There’s a nerve that makes your diaphragm move that they will cut to stop right half of his diaphragm from moving. There is also a large group of nerves that are surround by scar tissue that they want to try and remove because they believe it to have cancer cells still, but this nerve could be damaged and cause paralysis of his right arm. They are going to place a silicone implant to keep is heart from shifting. He said he could go in start surgery and have to stop because he sees things that they can’t on the images. We went over all the risks in great detail. He said again that this would be a life threatening surgery that he might not he might not survive but that he also has a life threatening tumor that if they don’t remove it, he might also no survive, so we had to make the difficult decision to trust in our surgeon that his plan for surgery was the correct plan for Christian and the right decision for his cure this time. Our surgeon told us that he will treat him like he is his own child. He will be in the icu for minimum four days and in hospital for 10-14 days at a minimum if everything goes well. The hospital has been very busy lately so they told us that there was a chance that they may not a room available for him in ICU after his surgery and in that case, they would move him across the street Corneal Hospital to recover in ICU, but they will still be his doctors there. The head of surgery will also be in the operating room to assist; he has been a pediatric surgeon for 50 years there. He is retired but still helps in cases like this. We knew that there was a lot of risk in performing this surgery and that it would take a very long time to perform. We got updates from the nurse in the OR room every few hours. When he could come of surgery and went to ICU, he was intubated on a ventilator. After surgery it is important we keep him moving and doing breathing exercises to keep the left lung strong. We must try to keep him from getting sick. The simplest thing like pneumonia could be fatal for him. He said this is the most serious surgery you can get. He said it will take probably three hours just to get into his chest with all the scare tissues from previous surgery. It will be an all-day surgery. The cancer could get used to the chemotherapy and mutate and not respond to chemotherapy. He will have one or two chest tubes. They will have to put in another line, like a chemo port line on the other side of his chest, incase he needs large doses of blood products, but it would come out before we leave the hospital. He will also have an epidural. May 22nd we were told that surgery was off for tomorrow. He went in at 8am for MRI and the team met with us about the pet scan from the day before. They said they found out late and it’s not something to talk about over the phone. They saw a spot on his spleen, and they think the cancer has spread. They are going to schedule a biopsy to see what exactly this spot is on his spleen. If it is PPB they won’t do surgery because they know it will just keep coming back and if they do surgery, they have seen kids stuck in the hospital till the end. It could be a different type of cancer because PPB normally spreads to the bones and the brain. Christian is going to be his first case tomorrow morning for a biopsy. The biopsy usually takes about hour with complications being that he can have excessive bleeding because the spleen is a very large blood organ. If that was to happen, they would have to take him into surgery to stop the bleeding. It would take about 3-4 days for the results to come back. May 23rd, he had the biopsy. By 10:40 he was in recovery and recovery about two hours long. They do that to make sure he not bleeding. It could be a cyst or an infection but the surgeon his 50 percent sure it’s cancer. After his biopsy today they went to the prom at the hospital. They hold a prom for cancer patients and siblings every year at MSK. They give out free dresses and t-shirts that look like suites. They have food, face painting, DJ and a photo booth. May 29th the results came in we were checking the portal constantly it came back benign but also said they may have not gotten the right spot so we will wait for the surgeon to call. The surgeon called today said he wants a bigger biopsy done just to make sure and he fells better that this one came back negative. He said to do another round of chemo than surgery in June. They will put him on the schedule unless someone cancels then they can do it sooner they are fully booked. He told us he knows we would do anything for Christian but same time reminded us on how risky this surgery will be. They scheduled the next biopsy for June 17th because they didn’t have nothing sooner available unless someone cancels. His next chemo would start on the 10th, and the last day of this cycle would be the day he has his biopsy so Rebeca is seeing if the medicine can be sent to her house this Saturday so he can start it this Monday, but the insurance company is giving a problem for the one medication. Our concerns are will he be well enough for the biopsy if he starts chemo and his counts are low as that can cause complications, so his oncologist is going to call us to discuss. All the back and forth with the insurance company, Rebecca was finally able to have the medicine sent to her house on Saturday so he could start on Monday. Sloan called and was able to reschedule his biopsy for June 6th. At this point the chemo medicine is already made, and it only last for a certain number of days, and he can’t start it because the chemo medicine must be giving at the same time every day. June 6th, he went in for the repeat biopsy. We were waiting for the anesthesiologist to come in the room to sign papers. Finally, he did and told us that someone had called out and they had to move everything around. They are intubating this time because he will have to be out longer than the first biopsy so they can take a larger sample of the possible tumor. The biopsy will be about an hour and then two hours recovery. Doctors called around 9:58 and said they don’t see anything on the ultrasound, and he had a colleague take a look just to make sure, but the spot was completely gone. This was such great news. They said just follow up with more scans. With the chemo medicine he on, he has to see the heart doctor every two months. June 12th, he started more chemo. Chemo would start at 9am and we would leave around 3-4 everyday. He scheduled for more scans on June 20th and if everything looks good surgery set for the 27th. All his scans are under anesthesia. June 20th, we went to Sloan for scans. His surgeon was not there so we went home and waited for them to call. With scans he recovers on the 9th floor. They only have two beds so as soon as they wake up, they come and get us to get him. They don’t require him to eat or drink before he can leave recovery. If he has an MRI or a procedure he recovers on a different floor and that’s one hour. With MRI or any scans that he gets nuclear meds, they will give a card saying how long he radioactive for. The nurse we talked to today went over what to expect with surgery next week. We read the report that came back in the patient portal it said the spot on his spleen was 0.6cm and the tumor grew in size. The tumor grew a decent size and it’s pushing on several organs, veins, his diagram, esophagus and vena cava vein. We are praying it hasn’t attached to any other parts where they can’t do surgery. We had faith today was going to be a good day and they wouldn’t see anything on his spleen and that the tumor didn’t grow but that was not the case. We are going to call and see if another doctor on the team can explain everything better. June 25th, we found out surgery is still on for Thursday. Arrival time is 6am and surgery at 7am.

June 27th one of the scariest days of our lives. They started surgery at 7:40. The first update call we got was that they were putting the epidural in and a central line and than surgery will start. We asked them to call with update every hour or sooner. We have had so many sleepless nights leading up to this point. This was by far one of the longest days of my life. They called again said they were putting in the other line in his neck and the surgery would start in about 40 minutes. They again called when they made the first incision. By 12:10 they started the resection. The next update call we got was that the tumor eroded to a main blood vessel, and they were working working on repairing that. Then they called said the tumor was out, but they had a lot more work to do. The next update we got was that he was going to start working on the bag around his heart. The nurse that calls is not in the actual OR room with him, but she calls as she gets updates. Another update at 3:07, he took out the rest of the lung completely on the right side, he had to take out a big part of his diaphragm that he was repairing now and then he will put the implant in and start to close him up. 6:39pm, he was in the ICU, and we were waiting to go see him. We talked to the surgeon, and he showed us the tumor he took out. At this point we think everything is ok and we received a call and were put into the room where you wait for the doctor to come in and talk to you. Time went by I kept asking what’s going on. Normally we wait like 5 mins for the surgery team to come and talk to us when we get put into more of these rooms, but it’s been almost 45 mins. The surgeon finally came and met with us and said he wasn’t sure why they put us in a room so early but he out of surgery and in the PICU. He said everything went as good as he hoped for. They were able to remove the tumor, the rest of his right lung and stapled the bronchial shut on the right side, removed a big piece of his diaphragm on the right side and repaired it with a patch. They had to remove a piece of the phrenic nerve that controls the diaphragm movement on that side. They had to repair a hole on the main artery that the tumor had eroded. They didn’t have to remove any of the bag around his heart, and they put in a silicone implant in his chest to prevent everything from shifting over from his left side. He could have a droopy eye but that can be dealt with down the road. While we were waiting upstairs in the waiting room, he stated having respiratory issues, so they had to rush to put the breathing tube back in and took him for CT scan, this was another heart stopping moment for all of us. They brought us into the recovery room and there were so many doctors and nurses around. He was responding to anyone, so they had us talk to him to try and wake him up to get him to respond. No words can describe this fear and pain. They had to get his breathing under control so they put the breathing tube back in and said we could see him in the next 30 minutes. We could not wait any longer to be with him. They did a CT of his brain after the breathing tube was back in. They were checking for cancer in the brain or seizures. He was barely responding or even moving. He can hear us they said that he is under a light sedation. They ruled out neurology issues for now. Even his surgeon was scared at this point. They will do nerve testing every hour. We haven’t seen him sense we got back from the CT scan. Panic is in full force. Our hearts break. The surgeon couldn’t believe how much the tumor grew in three months. Finally, we were able to go in and be with him he was squeezing my hand but still on the ventilator. Every hour we ask him to squeeze our hands and push his feet. They had to consistently suction him because he had a lot of blood in his mouth, and he was biting in the tube. I was so proud of our daughter at how brave and positive she stayed the entire time. They have to keep him sedated enough so he doesn’t take the breathing tube out but also will respond to us. They said he won’t remember most of this part from the anesthesia. He had a tube in his nose, one chest tub, the ventilator, a urine catheter, an artery iv in his foot, and his chemo port was still accessed. They take blood to read his oxygen levels so they can lower the oxygen in the ventilator, so he starts to breath on his own. We had a nurse outside our room that didn’t leave, and they checked him every hour. I did not sleep a wink; I just sat and held his hand all night. He also has an epidural in his spine that stays in until discharge. At 12 midnight they will check his CBC and eyes with the machine. They also check his eye with a light to see that his pupils dilate. 1:30am, they had to put in another breathing tube because the one he had wasn’t pulling back to suck the mucus out of his left lung. He started to to bleed in his mouth and was trying to cough. He keeps biting the piece of tube and that’s why it wouldn’t work. They gave him a heavier sleepy medicine. Then the surgeon said we will be in the PICU for a few more days, that he doesn’t want to take the ventilator out because he had three of them in the past 24 hours. They are still doing nerve checks every four hours instead of every hour. He’s responding for those. His machines were going off like crazy all night because of all the thick fluid in his left lung so they increased the oxygen. He lost a tooth during surgery so they did an x-ray this morning to see if they could see it. The surgeon said he had one of the biggest surgeries that they do at that hospital and had complications with in six hours he said it will be a long recovery. June 28th, they took the breathing tube out and we are moving in the right direction. He still on oxygen but breathing is a lot better. They took the central needle out of both of his feet and the NG tub out of his nose. He still has a lot more to take out, but this is a great start. He walked to the scale and sat on my lap in a chair. He is my cuddle bug, and it was so nice being able to hold him again. He has the epidural and gets pain meds around the clock but if he needs more, we can push a button. His pain tolerance is unreal, not just sayin this because he is my son, but he is truly a real-life superhero. Everything he has been through, and he has never complained. He still swollen and tired but doing great. Our goal is to get him up and moving to keep that left lung going with no problems. The doctors and nurses here are the best of the best. I know why people come from all over the world to come here. The tumor was so big to be in his little chest. I will never understand why kids get cancer. They won’t let Chris and Gabby stay the night. He can drink fluids at this time and hopefully get the catheter out tomorrow. They give him medicine to make him pee. They changed the bandage on his neck from that central line. June 29th, they took the urine catheter out, but he hasn’t peed yet. They want him eating and drinking but he’s not ready yet. By one in the afternoon, he went for two walks they took the line out of his neck. When they took the stitches out, he said that hurt so bad. His surgeon came in today on his day off just to see him. He still needs oxygen and the blood in his chest tub is getting lighter. When the nurse was taking the stitches out of his neck, she said he must be really special for the doctor to come in on his day off. We owe that man our lives, he has saved our sons life twice. He a true blessing. He had said that night things were goin downhill for what they thought the worse and that Christian likes to give him gray hair. It’s weird only seeing the left side of his chest move. Child life and a couple nurses had asked if we were going to write a book about his cancer journey. They tested the fluid in the plural wall that came back positive for PPB. June 29th 6:16 pm they put the urine catheter back in because he wasn’t peeing. They have him on light fluids, but his bladder is full. July1st he was doing good, no changes, they did a chest x-ray to see if there any changes in his left lung and if everything looks good, we will go to the other side to continue recovery in a regular room. Chest tub is still putting put a lot of fluid so that will stay in. He did drink last night but still not eating. The surgeon came in said he may go home on oxygen, that they are waiting to see the x-ray. He did smile today and did his cute face. July 2nd we were in a room with a window which was nice sense its shared rooms. He was eating, did five laps around the hallways. They took the oxygen off today. His oxygen levels dropped to in the 80’s, they shouldn’t be under 95. They are going to try to lower his fluids over tonight. I keep telling him he’s a superhero and he’s remarkable and amazing and that there are no words to explain how strong he is. He keeps saying you keep repeating yourself lol. I said Well its true and I want you to know how brave he is. July 4th, we watched fireworks from our room from a distance. July 5th, they took the chest tube out and the epidural. They took the urine catheter out too, so he has to pee on his own. He was coughing a lot. He did so good today we were able to go home and come back next week for a follow up. July 10th, we go next week to the Proton Center for a scan to make his mold for radiation, then two weeks after that, he will start his 20 days of proton radiation. All his radiation will be done under anesthesia. They will hit the entire interior of his right side of his chest. After radiation they will give him a different chemotherapy to start. His scans looked good so they will do full set of scans after radiation is done sometime in September. He has a little lean which is normal. It’s because of how many times they have cut his ribs open. Radiation hitting the tissue could make it worse. July 17th, we go tomorrow for the CT scan and to make an imprint mold of his body. Friday we will talk more with the oncologist to discuss this new chemo plan. What we know so far is it might be two chemo medicine five days, and they want to start Monday. He hasn’t been moving around much but we did go outside to play with some water balloon. July 18th, he started radiation at the Proton Center in the city. They have a big bell to ring in the lobby, I said I wish grandma was here so she could ring that bell with him. We had found out that the surgeon was texting the oncologist before the surgery making sure everyone was on board and if this was the right decision and the oncologist said yes this is what they want, they want the tumor to come out. He was second guessing the surgery because how risky it was. He is supposed to start the new chemo in two weeks, but we have to talk to the radiation doctor to make sure its ok because originally, she said no chemo while he is getting radiation. It’s two chemo medicine for five days and every three weeks. This is a bridge until radiation is done and more testing on the tumor is done. They talked with us about immunotherapy. They would test to see who the better match is Chris or myself. Long story short we decided not to go this route as it could make him very sick and the outcome may not be good.













July 18th was the first radiation treatment and the last was August 30th. He did amazing and all the nurses were great. During the last week of radiation, he also got a cycle of chemo. August 7th, he has to go to the hospital to get blood and platelet transfusion. August 12th, he has to go to the hospital to get blood and platelet transfusion. August 16th, he got radiation, and he has to go to the hospital to get blood and platelet transfusion. August 28th, he got radiation, and he has to go to the hospital to get blood and platelet transfusion. His new chemo plan included the following medicines, Cytoxan and Topotecan. These were giving through the chemo port, and he would also have a flush in between medicine. We would continue to give him the GCSF shots at home, typically once his counts began to drop from the chemo meds. Chemo medicine would be for five days, Monday through Friday. Then over the next two weeks he would continue to get bloodwork don to check his blood counts and would get platelets and red blood cells transfusion as needed. By the end of December, he started running fevers and we were in and out of the hospital and then we noticed blood in his urine, and he was having to pee every few minutes. We went to see the oncologist, and they did a urine test which came back positive for blood. They called an ambulance to transport him to the hospital across the street because he had a fever and the blood in his urine. Christian and I went by ambulance and Chris and Gabby met us there. We were admitted to the hospital where they ran bunch of tests and gave him fluids. He ended up being admitted for about three days. They said at this point they were sure it was a side effect from the chemo medicine. We went to a pediatric urologist, and they gave him medicine to stop his bladder from twitching, basically to stop him from feeling like he had to go pee so much. It was almost like a UTI side effect. That helped him big time. Talking to the oncologist we all decided not to continue with anymore cycles of chemo because there wasn’t any proof that more cycles would benefit his treatment over the number of cycles that h already received. He received 7 cycles of this chemo regimen. To finish the full set of cycles it would have been 12. Throughout his treatment, he still had to do continue to do scans. When chemotherapy was done, he had follow-up scans every three months. During his scans they did see some areas on the Pet/CT that were lighting up, but everyone thought these areas were scare tissue and nothing to worry about, so we stretched scans out to every six months. We could have had his chemo port removed but we wanted to keep it in this time. It felt like every time we had his chemo ports removed, on his next set of scans, the cancer would return. His last set of scans were on August 13th, at which time we found out he has a new tumor but now it is on the left lung. This nightmare feels like it will never end. No child should ever have to go through this. There must be more awareness, more people need to help spread the word so more people can help. Researchers need donations and funding to help find cures and better treatment options. Together, we can all come together to stop cancer in its tracks and come up with cures. Through it all, he has always been happy and full of energy. He is our world and there are no words to describe how devastating it is to hear the words, “Your child has cancer.” He has fought with love and support from everyone we know, and we are going to continue to fight this again and win! Not only is it heart breaking but it also makes you angry inside constantly wondering why this happened, how can we make him better, how can we help him become cancer free, how can we make sure this never comes back again. We have cried more during these past five years while he has been battling this cancer then ever in life. During all of this we also lost a lot of close people to us, my husband’s grandmother, then my dad, my mom, and even our dog Maximus. Anyone reading who knows someone who has been diagnosed with PPB cancer or any type of cancer for that matter, stay strong, keep faith and hope, and do your own research. Love them, be there for them, spend as much time with them, make as many happy memories as possible with them.





